Health
A more efficient health system benefits everyone, and is cheaper. Our goal is to reduce the health budget by 10% every five years, while improving all indicators of good outcomes (time on waiting lists, patient costs and so on).
A key to this is specialists, and not GPs. Your all-rounder doctor typically operates as efficiency as they can, and are reluctant to tell patients their problem cannot be fixed.
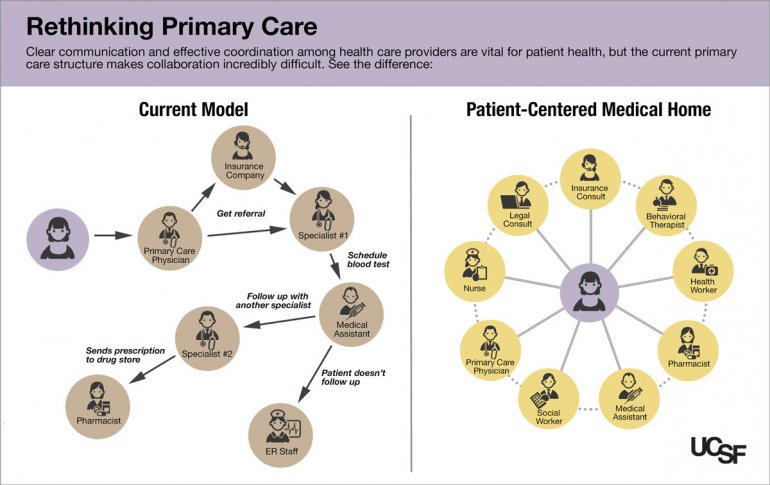
TEAM-BASED, COMBINED PRIMARY CARE
Australia has a serious obesity problem, which is reflected in the number of chronically ill people where obesity is a factor.
Rather than treating individual conditions – centres will be opened that specialise in combined conditions. For example, overweight people with musculoskeletal problems. They can see a knee specialist, a dietician, get blood work and physiotherapy in the one place, from one visit, with all specialists in close contact regarding the treatments. This is more convenient for the patient, and a team-based approach is more likely to succeed than seeing individual specialists separately over sometimes a long period of time. And because they are treating people with the same combination of conditions all the time, the specialists are going to become more skilled at treating combinations.
The other combination condition we would start with is heart disease, diabetes and obesity.
REFERRAL SYSTEM
If a patient has clear and obvious symptoms – say a knee injury or obesity – they should be able to book a specialist without a referral from a GP.
MID-LEVEL MENTAL HEALTH SPECIALISTS
A regular GP in a super clinic, who will have had no other consultations with a patient before of after, can diagnose and treat depression with medications that can have major impacts to a patient’s life. We recommend having specialist GPs for the diagnosis and treatment of mental health issues. So, not as specialises as a psychiatrist, but a doctor who will have a lasting relationship that monitors the patient.
EMERGENCY DEPARTMENTS
Too many people use emergency departments as a way of getting free, after hours treatment that would otherwise be better suited to visiting a GP.
We will introduce a $50 fee for all hospital emergency department treatments. And we will provide funding to subsidise late-night or 24 hour medical clinics, so that more will be available.
ANTIBIOTICS
The government knows all about this issue – see their Antimicrobial Resistance website – and is not enforcing the changes we need.
Wrongly prescribed antibiotics is a major threat to the life expectancy of all Australians, and potentially the biggest health risk the country will face this century.
Despite official guidelines to the contrary, GPs are prescribing millions of doses each year that will have no effect on the viral illnesses being treated. Expectations of patients are generally blamed.
We advocate that prescriptions that are contrary to official guidelines should be illegal, and doctors who do so can face serious consequences.
In combination with this, a public awareness campaign that clearly explains the key points be extensive and on-going, including substantial signage in medical centres.
But Why?
If antibiotic resistance continues, and superbugs become more commonplace, life expectancies can return to what we had in the 1800s, and people will be dying from very minor injuries, like a scratch.
PAIN KILLERS
Likewise, we are facing a major problem with the over-prescription of opioid pain killers. There is no action by the major parties, and it looks like (just in the USA), there won’t be until the death tolls are catastrophic.
Doctors feel obliged to provide solutions to patients. Saying there is nothing they can do to help does not seem to acceptable to them. Consequently antibiotics are prescribed for the common cold (even though it makes no difference), and opioids are prescribed as an easy fix to a complex issue: pain.
We will advocate for pain treatments centres, with specialists, for when the only solution to pain is pain killers. The specialists will work with patients to explore all possibilities, including over-the-counter medication and having no medication. They will also fully explain the risks of pain killers, especially the interactions with alcohol and other medicine.
They will not refuse opioids at the end of the process.
They will require follow up appointments.
HEALTH INSURANCE
80% of out-of-pocket expenses are via 7% of health professionals who grossly overcharge. Until now, how much these professionals charge has never been regulated. We would implement a maximum fee, for example 2x the scheduled fees. Not only will this reduce the overcharging, it would encourage patients to judge the healthcare in more ways than “most expensive is best”, while it has been proven that how much you pay has no bearing on results.
DENTAL
Nobody wants to go to the dentist. Not going to the dentist increases the odds of exponentially worse outcomes, which end up being addressed by public hospitals. There is a clear cost-benefit to providing free dental care for people below an income threshold. It would most likely be a tiered system like taxes – free for people under a particular income, partially paid for others, and not covered for the well off.